NAION Life!
NAION: Pathology & Neurology
ALERT!!!
It is absolutely critical to get immediate medical attention if you feel or sense any abnormality related to your eyes!
The Pathological part of a NAION Event
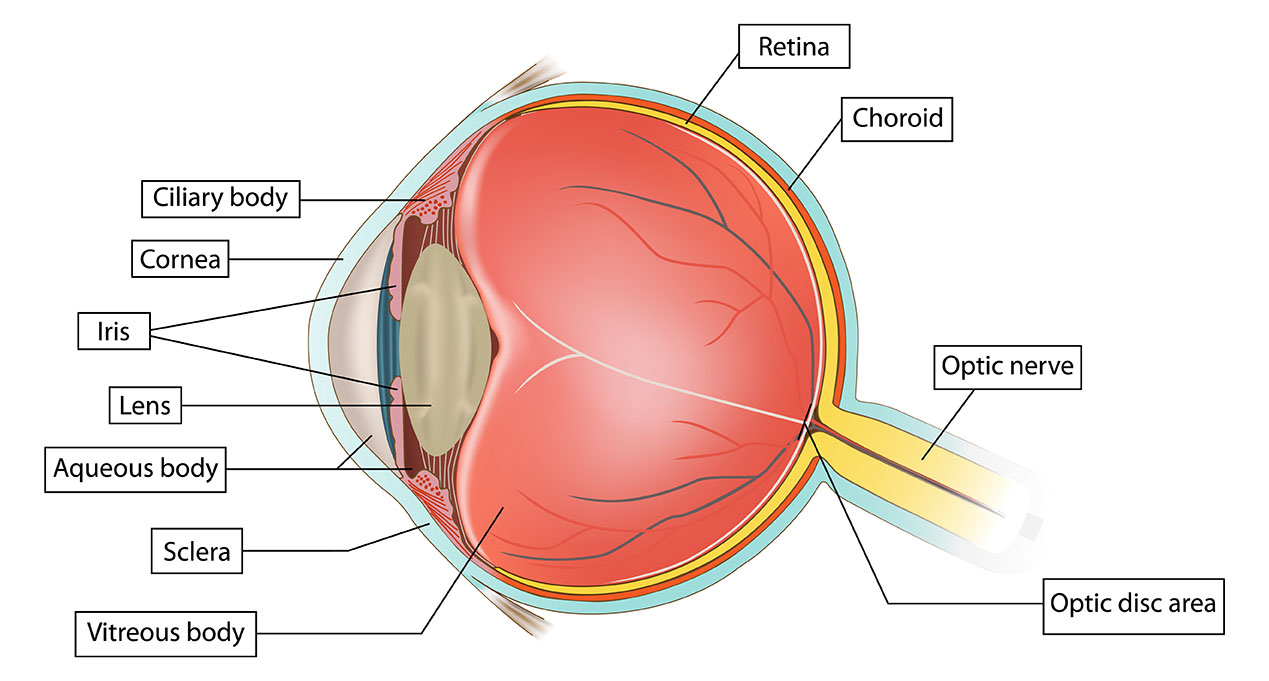
Non-arteritic Anterior Ischemic Optic Neuropathy (NAION) disrupts the vital role of the optic nerve, the pathway connecting your eye to the brain. This disruption, caused by interuption of blood flow, leads to sudden vision loss affecting one eye, a hallmark symptom of NAION. (It is unlikely but possible that another NAION event could affect the other eye)
There is rarely any pain associated with a NAION event and if vision loss is accompanied by pain there could be another reason and should be checked by a Neuro Ophthalmologist immediately. Vision loss may be gradual over hours or days and can be disorienting and lead to challenges with balance and coordination. This is because the brain relies heavily on visual information to navigate the environment.
Cause:
-
- NAION is caused by a sudden decrease in blood flow to the optic nerve head.
- This results in ischemia (lack of oxygen) to the anterior portion of the optic nerve, resulting further in various levels of irreversable nerve damage.
- Mechanism:
- The exact mechanism is not fully understood, but it’s believed to involve:
- a) Structural crowding of nerve fibers in the optic disc (Measured by Disc-to-cup ratio).
- b) Impaired autoregulation of blood flow to the optic nerve head.
- c) Nocturnal hypotension (low blood pressure during sleep).
- Risk Factors:
- Small optic disc with little cupping (“disc at risk” “crowded disc” disc-to-cup ratio). Imagine a very narrow passageway through the disc in which a blood vessel delivers blood and oxygen.
- Hypertension
- Diabetes
- Sleep apnea
- Hyperlipidemia (the presence of excess fat or lipids in the blood)
- Smoking
- Use of certain medications (e.g., PDE5 inhibitors like Viagra & Cialis) have been called into question regarding NAION
- Ozempic has been called into question regarding NAION
- Pathological Changes:
- Swelling of the optic disc
- Eventual atrophy of the optic nerve fibers
- Permanent loss of retinal ganglion cells ( the little nerve cells that branch off of the main optic nerves.)
- Clinical Presentation:
- Sudden, painless vision loss, often noticed upon waking but can happen at anytime.
- Altitudinal visual field defect (Vision above and/or below the horizon line)
- Reduced color vision (as if a gray cloud or veil covers shapes and colors)
- Distinction from Arteritic AION:
- NAION is not associated with giant cell arteritis, unlike its arteritic counterpart
- Prognosis:
- Generally poor for significant visual recovery
- Risk of recurrence in the same eye is low, but there’s a risk for the fellow eye
Understanding this pathology is crucial for diagnosis, management, and patient education. It’s important to note that while treatments are limited, addressing underlying risk factors can be beneficial.
The Neurological part of a NAION Event

The neurology related to NAION (Non-Arteritic Anterior Ischemic Optic Neuropathy) primarily involves the optic nerve and its associated structures. Here’s a breakdown of the neurological aspects:
- Optic Nerve Anatomy:
- NAION affects the anterior portion of the optic nerve, specifically the optic nerve head (optic disc).
- The optic nerve is composed of retinal ganglion cell axons that transmit visual information from the retina to the brain.
- Vascular Supply:
- The optic nerve head is supplied by the posterior ciliary arteries, branches of the ophthalmic artery.
- NAION results from compromised blood flow in this region.
- Neuronal Damage:
- Ischemia leads to damage and death of retinal ganglion cells and their axons.
- This results in irreversible vision loss.
- Visual Pathway Involvement:
- The damage occurs before the optic chiasm, affecting input from one eye.
- This results in monocular vision loss and can affect various parts of the visual field, often the inferior field.
- Pupillary Reflex:
- NAION typically causes a relative afferent pupillary defect (RAPD) in the affected eye due to decreased signal transmission along the affected optic nerve.
- Neurotransmitter Involvement:
- Glutamate excitotoxicity may play a role in the death of retinal ganglion cells during ischemia.
- Neuroplasticity:
- Some patients may experience limited visual improvement over time, possibly due to neuroplasticity and adaptation.
- Autonomic Nervous System:
- Dysregulation of the autonomic nervous system, particularly nocturnal hypotension, may contribute to the development of NAION.
- Central Nervous System Implications:
- While NAION primarily affects the optic nerve, it’s considered a warning sign for other vascular events in the central nervous system.
- Neurological Differential Diagnosis:
- NAION must be distinguished from other neurological conditions affecting the optic nerve, such as optic neuritis, compressive optic neuropathy, or arteritic anterior ischemic optic neuropathy.
- Neurodegenerative Considerations:
- Some research suggests a potential link between NAION and neurodegenerative diseases, though this connection is not fully established.
- Neuroimaging:
- MRI of the brain and orbits may be used to rule out other neurological causes of vision loss, though it’s typically normal in NAION.
Understanding these neurological aspects is crucial for accurate diagnosis, proper management, and potential development of neuroprotective strategies for NAION.
The above bulleted items were derived from a Claud AI query